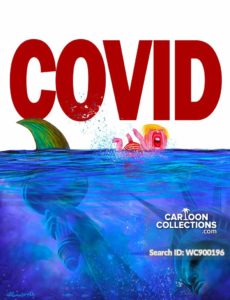
SCI-TECH MEDICINE: Covid-19 caused by a ‘smart’ virus that can find blind spots, crucial for system to be flexible to overcome challenges: Experts
SINGAPORE – Covid-19’s unique ability to both infect humans and cause disease means it is vital that the healthcare system be flexible enough to take on new challenges the “smart” virus poses, a panel of experts said on Wednesday (April 22).
Professor Dale Fisher, a senior infectious diseases expert at the National University Hospital (NUH), pointed to infections at nursing homes and dormitories: “I’m learning that this virus is really smart.
“It can find our blind spots, it can find vulnerable people, it can find areas where there’s high transmission, despite our efforts.”
.


SPACE RESERVE FOR ADVERTISEMENT
Prof Fisher was one of three experts who spoke with The Straits Times senior health correspondent Salma Khalik on The Big Story on how new information about the coronavirus was guiding Singapore’s response.
Prof Leo Yee Sin, executive director of the National Centre for Infectious Diseases, noted that while Singapore had learnt from dealing with Sars (severe acute respiratory syndrome) in 2003, no two outbreaks were alike.
“This is very, very different from Sars,” she said, pointing to differences in terms of the scale of infections and the way the disease manifested in patients.
.

“No matter what system we have put in place, the more important thing is that the entire system must be flexible and be ready to take on whatever challenge in whatever form and whatever shape.”
.

Prof Leo said it was important for the public to understand why the month-long circuit breaker period was being extended by a further four weeks from May 4.
“This is a very smart virus, it will find ways to remain in the human population. So it’s not a simple virus for us to deal with. There’s human-to-human transmission, it can transmit when we are not aware,” she said.
Prof Teo Yik Ying, professor and dean of the Saw Swee Hock School of Public Health at the National University of Singapore (NUS), said that while there have been encouraging signs that the circuit breaker period has been effective so far, the number of new cases has not fallen as quickly as expected.
.

The three-day average number of new community cases affecting those who live outside of dormitories has fallen from 48 at the start of the circuit breaker period on April 7 to around 25 over the past three days, he said.
.

“Based on those numbers, we know that the circuit breaker is effective… but I am actually a bit disappointed that the numbers have not fallen as low as we were expecting,” he added.
This points to “leakages” in the community, whether these involve people who venture out without taking the necessary precautions or essential staff who may have to go to work, Prof Teo added.
“This is why there is a need to perhaps step up the circuit breaker measures to now limit the definition of what is essential services and to further restrict the essential sectors a bit more,” he said.
.

POLICY IMPLICATIONS
The experts also noted that people will need to be prepared for changes in policies as new information about the coronavirus is uncovered by scientists around the world.
At the start of the outbreak, for example, only those who were unwell were asked to wear a mask. Now anyone caught in public without one faces a $300 fine.
Prof Teo said knowledge about the transmission of the Sars-CoV-2 virus, which causes Covid-19, has changed over the months.
Preliminary research in January found that it was unlikely that those without symptoms could be spreading the virus, he said. Now, there is evidence that asymptomatic infections were possible.
“What I’m trying to emphasise is that our knowledge about the coronavirus is changing all the time. And as countries start to learn more, our policies need to change accordingly.”
Policies should also be evaluated in the larger social context, such as the stage of the outbreak in society, and with considerations about the psychological effects of an action.
Prof Leo said the effectiveness of masks in preventing respiratory diseases, not just Covid-19 but even with influenza, has constantly been debated.
“But having a mask on carries a very different behaviour, connotations and meanings as well, that it constantly reminds us that we are in a very unusual period of time,” she said.
.

“I hope that those kind of notions will also help us to be able to fully understand the importance in terms of social responsibility.”
This goes beyond just putting on a mask, but also about etiquette: “Even in normal circumstances, if people do develop respiratory symptoms, it’s always good to put on a mask for personal and societal protection.
“It is exactly what we need from the entire society and community today to be together to fight Covid-19.”
.

TESTING MECHANISMS
There was also discussion about the two main types of tests being used around the world to determine if a person has been infected.
A virology test detects the presence of viral genetic material in a patient via a process known as polymerase chain reaction.
A serology test, however, tests for antibodies in the blood of people who have previously been infected, said Prof Teo.
Antibodies are produced by the immune system to fight an infection.
While serology tests are useful to find out how many people in the population have already been exposed and infected with the virus, they are not without flaws, he said.
“The issue with serology tests that governments worldwide right now are grappling with, including the World Health Organisation, is to what extent the presence of antibodies actually correlates with the immunity against reinfection,” noted Prof Teo.
The current evidence does not yet support the notion that those with antibodies are immune to subsequent infections, he added.
There have been reports that South Korea was seeing a growing number of recovered Covid-19 patients who relapse.
But Prof Leo said the scientific evidence is not robust enough to determine that those who have recovered from Covid-19 could be re-infected.
There are multiple possibilities why patients who have recovered test positive for the presence of the virus.
One, the ability to pick up the presence of a virus may last for a long time for many patients with respiratory disease infections.
“This is what we call viral shedding, and the shedding can go on for weeks and for months,” noted Prof Leo.
.

“Now, this does not represent that this person is still actively having the infection; it just means that the body is trying to take a period of time clearing the virus from the respiratory system.”
A second possibility is that patients with respiratory tract infections may take a while to fully recover.
“For example, a cough can be one of the last clinical symptoms to disappear from any patients with respiratory tract infections,” she said.
“So there is still a lot more that we need to learn. And I will say that this is a worldwide phenomenon.”
.


SPACE RESERVE FOR ADVERTISEMENT
.
.

All photographs, news, editorials, opinions, information, data, others have been taken from the Internet ..aseanews.net | [email protected] | For comments, Email to : The Scientist | Contributor